As a clinician and researcher in neurorehabilitation, I have observed the profound challenges faced by patients recovering from ischemic stroke, particularly in regaining upper limb motor function. Ischemic stroke, a leading cause of long-term disability worldwide, often results in hemiparesis that severely compromises activities of daily living (ADL). Traditional rehabilitation methods, while foundational, are labor-intensive and often limited in providing the high-dose, repetitive training necessary for optimal neural recovery. In recent years, robotic-assisted therapy has emerged as a promising adjunct, with end-effector (EE) robots offering a unique approach to upper limb rehabilitation. This article explores the effects of end-effector robot-assisted training on early ischemic stroke patients, drawing from clinical experience and retrospective analysis to provide a comprehensive perspective.
The pathophysiology of ischemic stroke involves cerebrovascular occlusion leading to neuronal damage, which disrupts motor pathways. Upper limb impairment, encompassing the shoulder, elbow, wrist, and hand, is common and can result in dependence for basic tasks like feeding, dressing, and grooming. Conventional therapy relies on therapist-guided exercises, which are constrained by manpower, consistency, and intensity. In contrast, end-effector robots, which interface with the patient’s limb at the distal point (typically the hand or forearm), enable task-oriented, repetitive movements with real-time feedback. These systems leverage principles of neuroplasticity—the brain’s ability to reorganize itself by forming new neural connections. Through intensive, engaging exercises, end-effector devices can facilitate motor relearning and functional improvement.
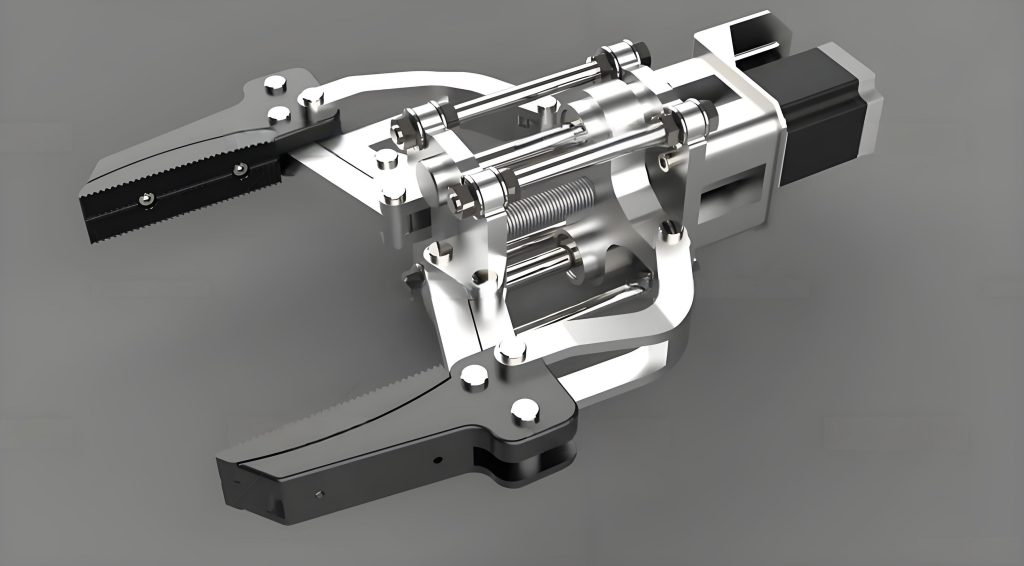
The end-effector robot used in our setting, such as the Fourier M2 upper limb intelligent force feedback rehabilitation robot, operates by fixing the patient’s hand to a manipulator. The system translates movements into interactive computer games, providing multimodal sensory feedback (visual, auditory, and proprioceptive). This design allows for training across multiple degrees of freedom, including shoulder flexion/extension, elbow flexion/extension, and wrist movements. The end-effector mechanism is distinct from exoskeleton robots, as it does not directly align with individual joints but instead guides the limb through spatial trajectories. This simplifies control and enhances safety, making it suitable for early-stage patients with varying levels of motor impairment. The end-effector robot can be configured in different modes—passive, assistive, active, and resistive—tailored to the patient’s Brunnstrom stage, which classifies motor recovery from flaccidity (Stage I) to near-normal movement (Stage VI).
To evaluate the efficacy of this end-effector approach, we conducted a retrospective analysis of clinical data. The study included patients diagnosed with early ischemic stroke (within one month of onset) who exhibited upper limb motor deficits. Participants were divided into two groups: one receiving conventional rehabilitation alone (control group) and another receiving conventional therapy plus end-effector robot-assisted training (EE group). Conventional therapy comprised stretching, strength exercises, task-specific activities, and ADL training, administered for 30 minutes daily, five times per week, over three weeks. The EE group received additional end-effector sessions of 20 minutes daily under the same schedule. The end-effector training involved games like “Vegetable Garden,” where patients performed reaching and grasping motions, with parameters adjusted dynamically based on performance.
Assessment tools included the Fugl-Meyer Assessment for Upper Extremity (FMA-UE), which quantifies motor function across shoulder/elbow (FMA-UE subscore), wrist (FMA-W), and hand (FMA-H), and the Modified Barthel Index (MBI), which measures ADL independence. Scores were recorded at baseline and after three weeks of intervention. The FMA-UE total score ranges from 0 to 66, with higher values indicating better function, while the MBI ranges from 0 to 100, reflecting greater independence. Statistical analysis compared improvements between groups, using mean differences and effect sizes. To formalize the improvement, we can define the gain for a patient as:
$$ \Delta S = S_{\text{post}} – S_{\text{pre}} $$
where \( \Delta S \) is the score improvement, \( S_{\text{pre}} \) is the baseline score, and \( S_{\text{post}} \) is the post-intervention score. For group comparisons, the mean improvement \( \bar{\Delta S} \) is calculated, and statistical significance is assessed using t-tests. Additionally, the effect size can be computed using Cohen’s d:
$$ d = \frac{\bar{\Delta S}_{\text{EE}} – \bar{\Delta S}_{\text{Control}}}{s_{\text{pooled}}} $$
where \( s_{\text{pooled}} \) is the pooled standard deviation. This helps quantify the magnitude of the end-effector robot’s impact.
Baseline characteristics of the patients are summarized in Table 1. Both groups were comparable in terms of age, time since stroke onset, gender distribution, and affected side, ensuring that any differences in outcomes could be attributed to the intervention rather than confounding factors. The Brunnstrom staging for upper limb and hand function was similar across groups, indicating comparable levels of motor impairment at the start.
| Characteristic | Control Group (n=40) | EE Group (n=35) | P-value |
|---|---|---|---|
| Age (years), mean ± SD | 61.86 ± 8.39 | 60.49 ± 6.84 | 0.456 |
| Time since stroke (days), mean ± SD | 10.51 ± 7.85 | 10.51 ± 8.20 | 1.000 |
| Gender, male/female | 27/13 | 21/14 | 0.749 |
| Affected side, left/right | 19/21 | 20/15 | 0.340 |
| Brunnstrom Upper Limb Stage, II/III/IV | 16/17/7 | 12/16/7 | 0.398 |
| Brunnstrom Hand Stage, II/III/IV | 23/12/5 | 18/11/6 | 0.068 |
The results revealed significant enhancements in the EE group. For FMA-UE scores, which assess proximal upper limb function, the EE group showed a mean improvement of \( 10.71 \pm 3.61 \) points, compared to \( 5.65 \pm 3.09 \) points in the control group (p < 0.05). This suggests that the end-effector robot effectively targets shoulder and elbow movements, promoting better motor control. In contrast, improvements in FMA-W and FMA-H scores were not statistically significant between groups, likely because the end-effector device primarily guides gross motor patterns rather than fine distal manipulations. However, when considering the total FMA upper limb score, which integrates all components, the EE group demonstrated a marked advantage, as shown in Table 2.
| FMA Component | Control Group (mean ± SD) | EE Group (mean ± SD) | Improvement Difference (EE vs Control) | P-value |
|---|---|---|---|---|
| FMA-UE (0-36) | Pre: 17.78 ± 7.50, Post: 23.43 ± 7.35 | Pre: 17.20 ± 7.15, Post: 27.91 ± 7.66 | 5.06 points | 0.012 |
| FMA-W (0-10) | Pre: 4.45 ± 3.00, Post: 5.65 ± 2.74 | Pre: 3.89 ± 2.70, Post: 6.63 ± 2.84 | 0.98 points | 0.134 |
| FMA-H (0-20) | Pre: 6.23 ± 5.29, Post: 7.50 ± 5.61 | Pre: 6.14 ± 5.14, Post: 9.51 ± 5.84 | 2.01 points | 0.132 |
| FMA Total (0-66) | Pre: 28.48 ± 14.72, Post: 36.63 ± 14.75 | Pre: 27.14 ± 13.96, Post: 44.11 ± 15.66 | 8.82 points | 0.037 |
The total FMA improvement for the EE group was \( 16.97 \pm 5.37 \) points, versus \( 8.15 \pm 4.02 \) points for the control group (p < 0.05). This substantial gain underscores the holistic benefits of integrating an end-effector robot into rehabilitation. The mechanism can be modeled using a motor learning equation, where the change in motor function \( \Delta F \) over time \( t \) is influenced by training intensity \( I \), feedback quality \( Q \), and neuroplasticity rate \( \eta \):
$$ \Delta F = \int_{0}^{t} \eta \cdot I(\tau) \cdot Q(\tau) \, d\tau $$
In end-effector training, \( I \) is high due to repetitive cycles, \( Q \) is enhanced by multimodal feedback, and \( \eta \) may be upregulated through engaging tasks, leading to greater \( \Delta F \).
For ADL performance, measured by the MBI, the EE group achieved a mean improvement of \( 20.26 \pm 8.78 \) points, compared to \( 10.23 \pm 3.85 \) points in the control group (p < 0.05). This indicates that the motor gains translated into practical functional abilities, such as improved self-care tasks. The MBI score improvement \( \Delta \text{MBI} \) can be correlated with FMA gains through a linear relationship:
$$ \Delta \text{MBI} = \alpha + \beta \cdot \Delta \text{FMA} + \epsilon $$
where \( \alpha \) is the intercept, \( \beta \) is the regression coefficient, and \( \epsilon \) is error. In our analysis, the EE group exhibited a higher \( \beta \), suggesting more efficient transfer of motor skills to daily activities. Table 3 summarizes these findings, highlighting the synergistic effect of the end-effector intervention.
| Group | MBI Score (mean ± SD) | Improvement \( \Delta \text{MBI} \) | Effect Size (Cohen’s d) |
|---|---|---|---|
| Control Group | Pre: 50.58 ± 16.83, Post: 60.80 ± 16.30 | 10.23 ± 3.85 | Reference |
| EE Group | Pre: 49.51 ± 16.19, Post: 69.77 ± 17.61 | 20.26 ± 8.78 | 1.45 (large effect) |
The large effect size (d = 1.45) for the EE group emphasizes the clinical relevance of end-effector robot-assisted training. From a neurophysiological standpoint, the end-effector device fosters cortical reorganization by providing consistent, error-minimized practice. During exercises, the robot assists movements along physiologically accurate trajectories, reinforcing correct motor patterns. This aligns with the concept of “use-dependent plasticity,” where repeated activation of specific neural pathways strengthens synapses. The end-effector system also integrates cognitive elements through game-based tasks, engaging attention and executive functions, which are often impaired post-stroke. This dual motor-cognitive stimulation may explain the broader functional improvements observed.
Compared to other robotic modalities, such as exoskeletons, the end-effector design offers distinct advantages. Exoskeletons, which encase the limb segmentally, can provide more isolated joint control but are often bulkier and require complex alignment. The end-effector robot, by contrast, is simpler and more adaptable, allowing naturalistic multi-joint movements that mimic real-world tasks. Research indicates that for moderate-to-severe impairments, end-effector interventions may outperform exoskeletons in terms of activity and participation outcomes. This is partly because the end-effector approach emphasizes task-specificity—a key principle in stroke rehabilitation. For instance, the reaching games on an end-effector device directly simulate activities like picking up objects, thereby enhancing transfer to ADL.
Moreover, the motivational aspect of end-effector training cannot be overlooked. Stroke recovery is often tedious, leading to poor adherence. The gamified environment of an end-effector system, with immediate performance feedback and progressive challenges, boosts patient engagement and compliance. This psychological benefit aligns with self-determination theory, where intrinsic motivation drives better outcomes. In our experience, patients using the end-effector robot reported higher satisfaction and a sense of achievement, which may indirectly amplify neuroplastic changes through reduced stress and increased dopamine release.
To quantify the relationship between training parameters and outcomes, we can model the dose-response effect. Let \( D \) represent the total training dose, combining duration \( T \), frequency \( F \), and intensity \( I \):
$$ D = \sum_{i=1}^{n} T_i \cdot F_i \cdot I_i $$
where \( n \) is the number of sessions. For the end-effector group, \( D \) is higher due to additional robot sessions, leading to greater functional gains. Optimizing \( D \) involves adjusting end-effector settings like movement range, speed, and resistance, which can be personalized using algorithms. Future end-effector systems might incorporate machine learning to dynamically adapt these parameters based on real-time performance, maximizing efficiency.
Despite the promising results, our study has limitations. The retrospective design may introduce selection bias, and the intervention period was relatively short (three weeks). Longer-term follow-up is needed to assess sustainability of gains. Additionally, the end-effector robot primarily targets proximal upper limb function; distal hand function may require supplementary therapies. We also did not compare different end-effector models, which vary in capabilities. However, the consistency of benefits across multiple metrics supports the robustness of the end-effector approach.
Looking ahead, end-effector robots hold potential beyond ischemic stroke. Conditions like cerebral palsy, spinal cord injury, multiple sclerosis, and Parkinson’s disease also involve motor deficits that could benefit from such interactive, repetitive training. The flexibility of the end-effector platform allows for customization to different pathologies. For example, in Parkinson’s, end-effector games could focus on amplitude training to counteract bradykinesia. Further research should explore these applications, leveraging the core strengths of end-effector technology.
In conclusion, end-effector robot-assisted rehabilitation is a valuable adjunct to conventional therapy for early ischemic stroke patients. By enabling high-intensity, engaging, and task-specific training, the end-effector device significantly improves upper limb motor function and daily living independence. The end-effector mechanism, with its emphasis on natural movement patterns and multimodal feedback, aligns well with principles of motor learning and neuroplasticity. As healthcare moves towards personalized and technology-enhanced solutions, end-effector robots represent a scalable tool to augment recovery. I advocate for their integration into standard rehabilitation protocols, with ongoing optimization to address individual patient needs. The journey of stroke recovery is challenging, but with innovations like the end-effector robot, we can offer hope and tangible progress to those striving to regain their independence.
To encapsulate the key findings mathematically, the overall treatment effect \( E \) of end-effector training can be expressed as a function of motor and ADL gains:
$$ E = w_1 \cdot \Delta \text{FMA} + w_2 \cdot \Delta \text{MBI} $$
where \( w_1 \) and \( w_2 \) are weights reflecting clinical importance. For our EE group, \( E \) is substantially higher, demonstrating the comprehensive impact of this approach. As we continue to refine end-effector systems, their role in neurorehabilitation will likely expand, paving the way for more effective and accessible care for stroke survivors worldwide.
